Perforated Ulcers
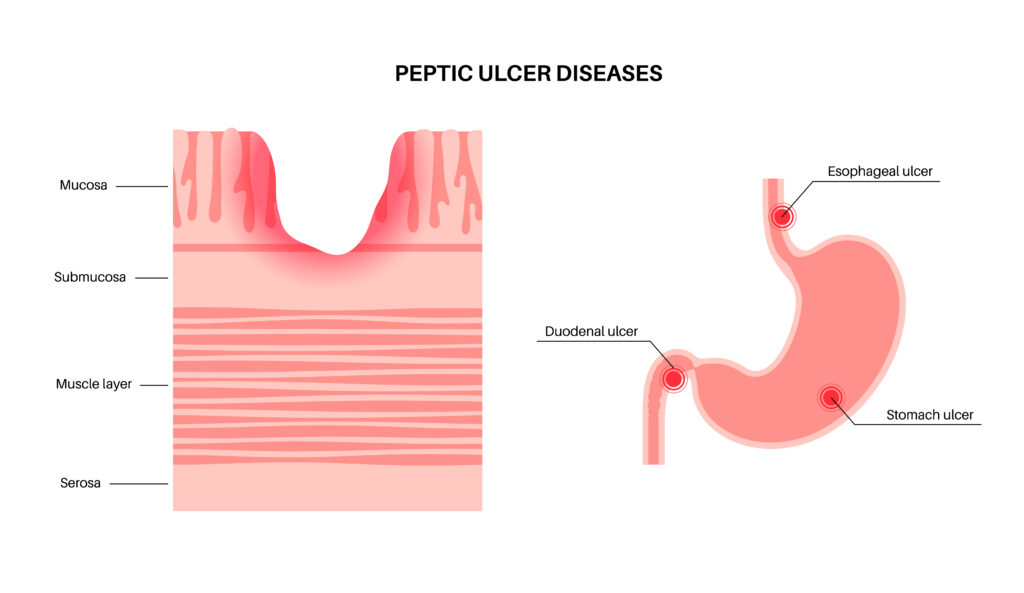
Perforated ulcers are a serious complication of peptic ulcers, which are open sores that develop on the lining of the stomach, small intestine, or esophagus due to erosion by stomach acid and digestive juices. At Brundavan Nursing Home, we recognize the urgency of diagnosing and treating perforated ulcers promptly to prevent life-threatening complications such as peritonitis (inflammation of the abdominal cavity) and sepsis. Our approach to perforated ulcers involves rapid assessment, surgical intervention, and supportive care to ensure the best possible outcomes for our patients.
Clinical Evaluation: We prioritize early clinical evaluation and diagnosis of perforated ulcers in patients presenting with symptoms such as sudden, severe abdominal pain, nausea, vomiting, fever, and abdominal tenderness. Our healthcare providers conduct a thorough medical history review, physical examination, and diagnostic tests such as abdominal imaging studies (X-rays, CT scans) to confirm the diagnosis of a perforated ulcer and assess for signs of complications such as free air or fluid in the abdomen.
Surgical Intervention: Perforated ulcers require emergent surgical repair to close the perforation, remove any infected or necrotic tissue, and address any associated complications such as peritonitis or abscess formation. We offer prompt surgical intervention, typically performed using minimally invasive laparoscopic surgery or open surgery, depending on the patient’s clinical presentation, severity of the perforation, and surgeon’s preference. The goal of surgery is to achieve complete closure of the perforation and restore the integrity of the gastrointestinal tract.
Intravenous Antibiotics: In addition to surgical intervention, we administer intravenous antibiotics to patients with perforated ulcers to prevent or treat infection and reduce the risk of complications such as sepsis. Antibiotic therapy is initiated promptly after diagnosis and may be adjusted based on culture and sensitivity results to target the specific bacteria causing the infection.
Fluid and Electrolyte Management: Patients with perforated ulcers may experience fluid and electrolyte imbalances due to vomiting, diarrhea, or sepsis. We provide aggressive fluid resuscitation and electrolyte replacement therapy as needed to restore normal fluid balance, maintain hemodynamic stability, and support organ function during the acute phase of treatment.
Pain Management: We prioritize effective pain management for patients with perforated ulcers to alleviate discomfort and promote comfort during the recovery process. We offer multimodal pain management strategies, including intravenous analgesics, nonsteroidal anti-inflammatory drugs (NSAIDs), and patient-controlled analgesia (PCA) pumps, tailored to each patient’s individual needs and medical condition.
Nutritional Support: Adequate nutrition is essential for healing and recovery in patients with perforated ulcers. We provide enteral or parenteral nutrition support as needed to meet the patient’s nutritional requirements and promote wound healing, particularly in cases where oral intake is limited due to surgery or gastrointestinal dysfunction.
Postoperative Care and Monitoring: After surgical repair of a perforated ulcer, we provide comprehensive postoperative care and monitoring to assess the patient’s recovery, monitor for signs of complications, and facilitate early mobilization and ambulation. We closely monitor vital signs, laboratory parameters, wound healing, and bowel function, adjusting treatment as needed to optimize outcomes and prevent recurrence.
Long-term Management: Following recovery from perforated ulcer repair, we offer long-term management and follow-up care to address underlying risk factors such as Helicobacter pylori infection, nonsteroidal anti-inflammatory drug (NSAID) use, smoking, alcohol consumption, and stress. We provide patient education on lifestyle modifications, medication adherence, and preventive measures to reduce the risk of recurrent ulcers and complications.
At Brundavan Nursing Home, we are committed to providing timely, compassionate, and evidence-based care for patients with perforated ulcers. Our multidisciplinary team of surgeons, anesthesiologists, critical care specialists, nurses, and support staff work collaboratively to deliver safe, effective, and personalized care, ensuring that patients receive the highest standards of treatment and support throughout their recovery journey.
